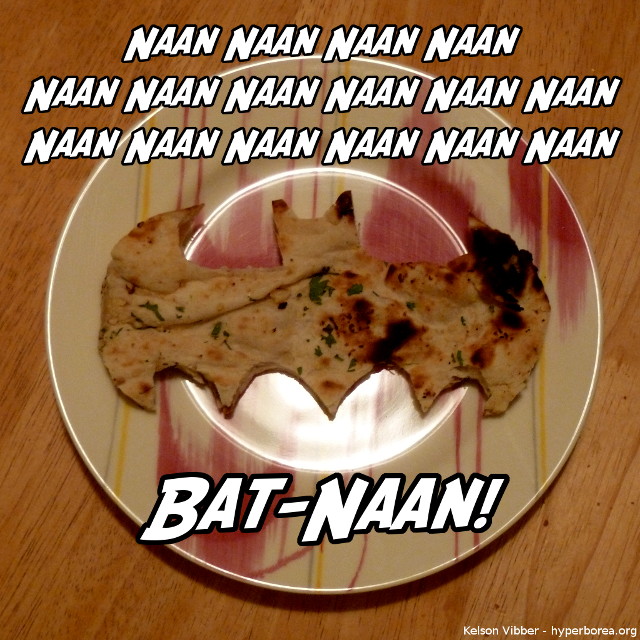
So, we were telling J to be careful of the “hot naan,” at which point I started singing “Hot naan! Hot naan! Hot naan!” Katie decided it needed to be bat-ified.
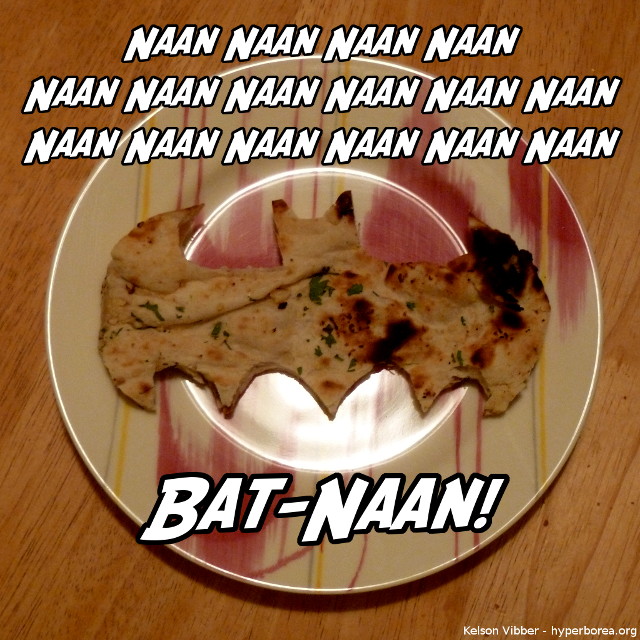
So, we were telling J to be careful of the “hot naan,” at which point I started singing “Hot naan! Hot naan! Hot naan!” Katie decided it needed to be bat-ified.
You’ve got to love this headline: Giant goat-cheese fire closes Norwegian roadway for six days. Apparently, brunost burns really well, and when a truck carrying it caught fire in a tunnel, responders were unable to get to it for days.
(Incidentally, the stuff is also really good. My family discovered it on a vacation to Disney World, of all places, where they served it in the smorgasbord at the Norwegian restaurant in Epcot.)
This is even weirder than the truck full of meat that caught fire on the 5 near Camp Pendleton a few years back, blocking the entire freeway in an area with no alternate routes for most of the day and stranding all of the Orange County & Los Angeles people trying to get to the first day of Comic-Con.
I’m going to have to start using “flaming goat cheese on a truck!” as a pseudo-curse.
Allergic Living reports on a peanut allergy treatment study that shows a great deal of promise. Called sublingual immunotherapy, or SLIT, it’s surprisingly simple: Introduce a small amount of peanut protein in drops beneath the tongue each day, slowly ramping it up over time.
After 44 weeks of the daily doses, 70 percent of those getting the peanut powder could tolerate at least 10 times more peanut in an oral food challenge before showing symptoms than they could have at the outset of the study. In a follow-up challenge at 68 weeks, they could tolerate about twice as much again.
It’s a similar premise to allergy shots, which work well for airborne allergens but not for food. And while I’m creeped out by the idea of deliberately ingesting something that I’m used to avoiding because it could kill me (this has to be done under medical supervision!), like so many other things it’s all about dosage. It makes sense that it could work.
The main drawback is that 30% of the participants didn’t show improvement, though the people running the study suspect that it’s a matter of finding the right dosage for each patient.
The article mentions another problem being that the amount tolerated is relatively small: they could eat the equivalent of two peanuts before experiencing allergy symptoms.
I say: Two peanuts? Are you kidding me? I would LOVE to be able to safely eat that much!
So it’s not enough to eat Thai food or PBJ. It would mean I can stop worrying so much about cross-contamination! I’d still carry my epi-pen around, but I’d feel a lot safer about, say, drinking a milkshake at a restaurant that also serves peanut butter shakes, or eating an eggroll at a place that also has kung pao, or eating a chocolate chip cookie that’s been stored on the same shelf as the peanut butter cookies.
One question I do have is how effective it is at reducing sensitivity to similar allergens. Would taking the peanut treatment help someone tolerate legumes better, or are they different enough to require a separate course of treatment?

The Walk for Food Allergy that I’ve been plugging over the last couple of months was held this Sunday. We drove out to Long Beach to join several hundred other people in the walk to raise funds for the Food Allergy and Anaphylaxis Network. You helped us raise $1,342.15, putting our team into the top 5, and the event overall raised $45,360 before offline donations are counted. The money goes to FAAN and their mission to support food allergy research, education, awareness and advocacy. FAAN sponsors a series of these events throughout the year, so if you’d still like to make a donation, you can contribute through December 31.

Because food allergies are on the increase, a lot of the people affected by them are children, so there were a lot of families at the event. I remember last year featuring a stage and information booths for support groups, medical groups and allergy-friendly food companies like SunButter and Enjoy Life. This year they also had an inflatable slide and a rock climbing wall. (The organizer said that they moved it to Long Beach so that they could get that wall.)
If you have food allergies, dining out is always a risk. We had a close call our first night in Chicago on a family vacation last month.
After a long day of travel, we got settled into our hotel room and went down to one of the hotel restaurants for a late dinner. It was a Sunday evening, around 9:30, and while the front desk had assured us that the restaurant was open until 11, that turned out to only be half true. The restaurant entrance was blocked off, but the kitchen was serving the full menu to a shared seating area that you entered through the bar.
We’d been concerned about finding food for our not-quite-two-year-old son. Kids’ menus are awfully limited these days, and very heavy on cheese, which he can’t eat. Chicken nuggets are fine once in a while, but only go so far on a ten-day trip. So we were pleasantly surprised to see a Sunbutter, jelly and banana sandwich on the kids’ menu. Because of my severe peanut allergy, we keep peanuts out of the house, so Katie goes to sunflower seed butter and almond butter for toast and sandwiches, and J loves it so much he’ll demand a taste if she’s eating it. Score!
After a very long wait, the waitress finally brought the sandwich, dropped it off saying, “Here’s your PBJ,” and left.
Wait, PBJ?
Katie tasted it, and it was in fact peanut butter.
Red alert mode engaged!
As I mentioned, I’m severely allergic to peanuts. We don’t know yet whether J is, but we didn’t want to risk finding out in a hotel in a strange city thousands of miles from home.
The waitress seemed a bit confused by the issue when we finally got her attention (all the while trying to find other things we could feed an increasingly-cranky toddler who thought he was finally going to eat), and we had to point out that yes, the menu specifically said Sunbutter.
They did take the sandwich off the bill, and replaced it with a plain jelly-and-banana sandwich. But it put us on alert for the rest of the week.
The really disturbing thing was that it wasn’t just any sunflower seed butter listed on the menu, but a specific brand, one whose purpose is to be a safe alternative for people who are allergic to peanuts. That’s like telling a diabetic that you have Clemmy’s sugar-free ice cream and handing them Ben and Jerry’s. Or giving someone Everclear to help with their dehydration.
We lucked out, because Katie caught it before J could eat any of it. Really, the restaurant dodged a bullet too: They could have served it to a family with a confirmed allergic child. Imagine how blindsided they’d be when someone silently replaced a peanut-free food with peanuts. Continue reading
Someone once asked me if my food allergies — the ones that require me to carry emergency medication so that I can keep breathing if I eat something with peanuts — could be all in my head. I pointed out that they can be diagnosed by a blood test, and asked how my head could influence the results of a test on a vial taken to a lab three states away.
Allergies to nuts, grains, vegetables, seafood and milk are common. Allergies to meat? Much less so. But that’s starting to change.
A few months ago I read about adults (author John Grisham in particular) developing an allergy to red meat after being bitten by ticks.* And not just a low-level allergy like your face turning red — we’re talking full-on hives and anaphylactic** shock, the kind of thing that requires you to carry an Epi-Pen to make sure you keep breathing long enough to reach the emergency room.
Researchers have determined that the lone star tick’s bite can cause the body to produce an IgE antibody for a sugar called alpha-gal, which is found in mammal meat.
The result: from then on, you’re allergic to meat.
CNN calls it mysterious. Allergic Living calls it baffling. It’s certainly weird compared to “usual” allergies, and the fact that the reaction is usually delayed by a few hours makes it hard to diagnose, but we’re ahead of the game in understanding it: Unlike most allergies, we know what causes this one.
With most allergies, we know the process, but we don’t know what gets the ball rolling to begin with. We know that in people who are allergic to a food, exposure to it causes an IgE antibody reaction that triggers a massive release of histamines that sends the body into some level of shock, but we don’t know why some people have that reaction and others don’t.
There are a lot of ideas being investigated, with varying amounts of supporting evidence, but there’s still nothing we can point to and say: “This caused you to be allergic to nuts” or “That caused you to be allergic to milk.” Advice to parents concerned about keeping their child from developing allergies is all over the map.
When I posted this back in 2012, I segued into a call for fundraising for research. The particular fundraiser has since been discontinued, but research has dramatically improved both medical understanding and practical actions around allergies.
First: it’s been clearly demonstrated that early introduction of a food lowers the risk of a child developing an allergy to it. It’s not a guarantee, but at least there’s clear advice to parents now!
Plus, immunotherapy and IgE-targeting treatments can reduce sensitivity and severity (though they can’t always eliminate reactions entirely) for those of us who already have severe allergies, those who develop allergies as adults, and the (much smaller!) percentage of children who still develop food allergies even with early exposure.
Unfortunately there’s still no clear explanation for why that ~3% of children who do have early exposure still go on to develop allergies — or why some people bitten by the lone star tick develop what is now called alpha-gal syndrome and others don’t.
Advice these days is basically: Try not to get bitten by ticks, and if you do develop the allergy, stop eating red meat.
*Naturally, this was a few days after I hiked a severely overgrown trail without taking precautions against ticks, so I freaked out a bit, but I also hadn’t found any ticks when I got home from the hike.
**Fun fact: Chrome’s spell-checker doesn’t know “anaphylactic,” and suggested such helpful alternatives as “intergalactic” and “anticlimactic.” Not sure about the former, but I get the impression a lot of viewers suffered “anticlimactic shock” when watching the Lost finale.